An IRD diagnosis doesn’t change who you are.
Receiving a clinical diagnosis of an IRD such as retinitis pigmentosa, Usher syndrome, or Stargardt disease can be overwhelming. Whether you think you might have an IRD or you’re looking for information after a confirmed diagnosis, you are bound to have a lot of questions.
We hope to provide you with some answers and make the process of learning about IRD as easy as possible. But remember, an IRD doesn’t change who you are. Living with an IRD is about taking steps towards your goals and making adjustments along the way.
About IRD
Learn about rare inherited diseases that affect the retina and cause vision loss.
What is inherited retinal dystrophy (IRD)?
You might be wondering what IRD is, where it comes from, and what having an IRD will mean for you. This website is here to guide and support you.
So, what is IRD?
IRD is used to describe a collection of rare eye problems that are passed down from parents to children in the genes. IRDs are sometimes also called inherited retinal diseases or inherited retinal degenerations.1
There are lots of different types of IRD. Some names of the more common ones are retinitis pigmentosa (RP), Usher syndrome, Leber congenital amaurosis, and Stargardt disease, all of which you can find more information on here.
People with IRD have a mutation in one of the genes responsible for the function of the light-sensitive (photoreceptor) cells in the retina at the back of the eye. In IRD, these cells begin to stop working, work less effectively, or die, leading to a gradual loss of vision and blindness.1
It is important to remember that you are not alone in this. There are people of all ages living with an IRD, and it is the main cause of vision loss in people aged 15 to 45 years as well as a common cause of vision problems in children. Although rare, it has been estimated that IRD affects more than 2 million people worldwide (about 1 in every 2000).2
How different types of IRD affect the vision, symptoms and progression of these diseases are all different. This is because there are so many different types of IRD.
A quick guide to the retina
Retina: the back surface of the eye made up of two layers, full of cells that detect light (photoreceptor cells) and send signals to the brain to create images. Contains two types of photoreceptor cells: rods and cones.1
Macula: the most light-sensitive part of the retina, densely packed with photoreceptor cells, a central spot that is responsible for colour vision.1
Rod cells: mostly found around the edge of the retina, these cells are the ones that work in dim light and that help us see things that aren’t straight ahead.1
Cone cells: concentrated in the centre of the retina and mostly involved in seeing colour and give us detailed vision.1

Gene mutations and IRD
Learning about IRD in more detail can equip you with a better understanding of your condition and help you come to terms with your diagnosis.
All forms of inherited retinal dystrophy are caused by mutations in genes. These genes are involved in the development and function of light-sensitive cells (photoreceptors) and other cells in the retina.1
More than 260 genes have been associated with IRD, and a genetic diagnosis can be found in about 60% of all cases of IRD.3,4
Some types of IRD are caused by a single mutation in an identified gene, whereas others can be caused by lots of different mutations but are known by the same name.2 For example, Stargardt disease is usually caused by a mutation in a gene called ABCA4, whereas we know of mutations in 84 different genes that can cause retinitis pigmentosa.2
In some cases the genetic mutation that causes an IRD isn’t yet known, but research is always being done to discover more. Genetic testing can confirm a genetic basis for your disease and may determine what mutation is responsible for your particular IRD and what your options are.
Common genetic terms
Medical language can feel very jargon heavy and full of words you may not understand. Here, are some of the most common words with quick definitions to make things easier.
-
Chromosomes: tight bundles of DNA in the nucleus of cells that store the genetic information of an organism. Humans have 23 pairs of chromosomes with half of each pair coming from each parent
-
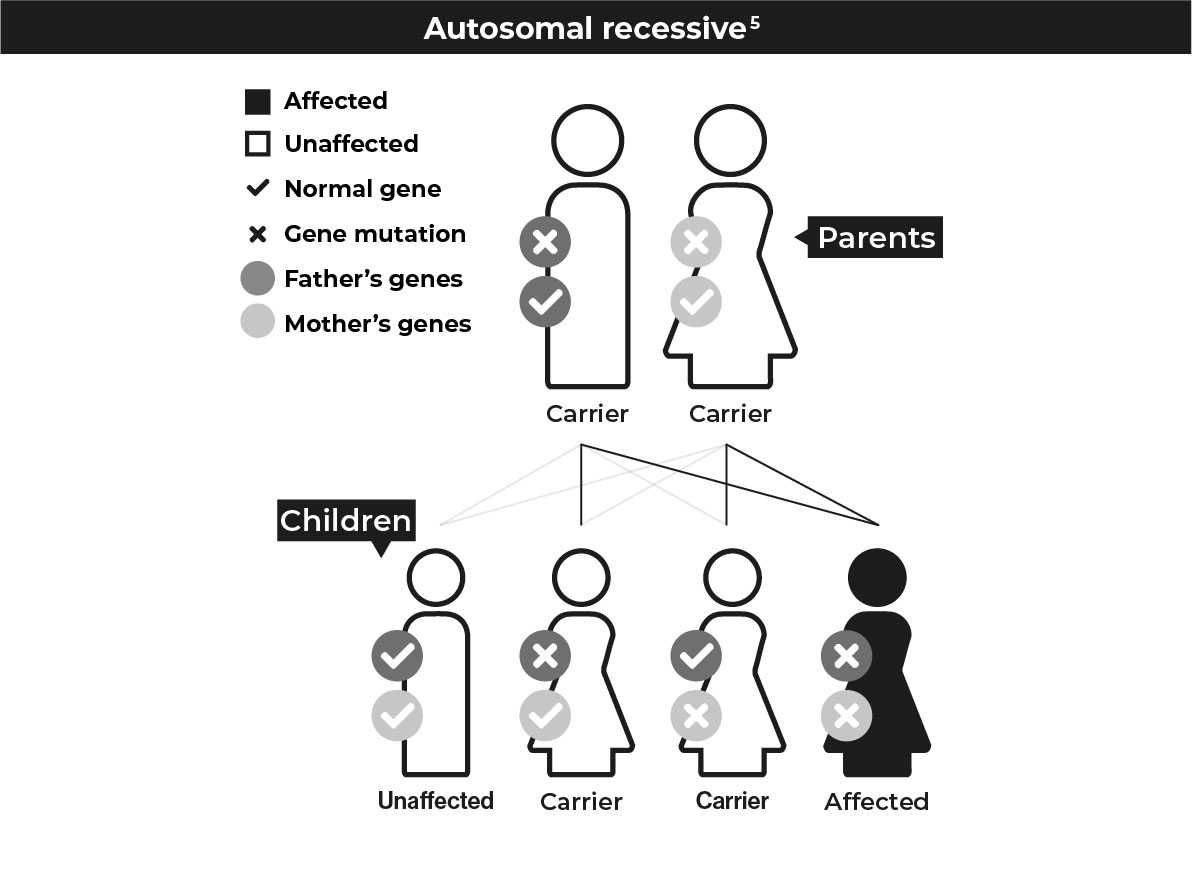
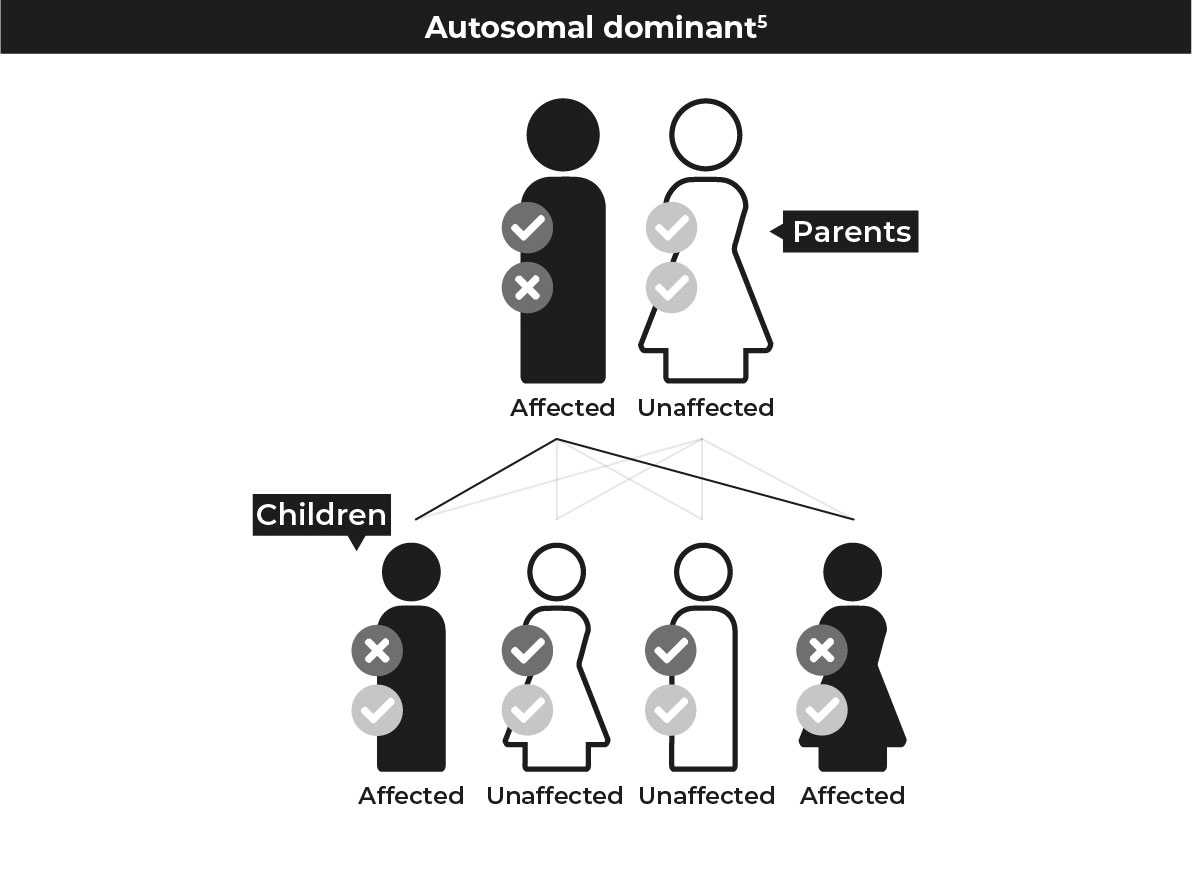
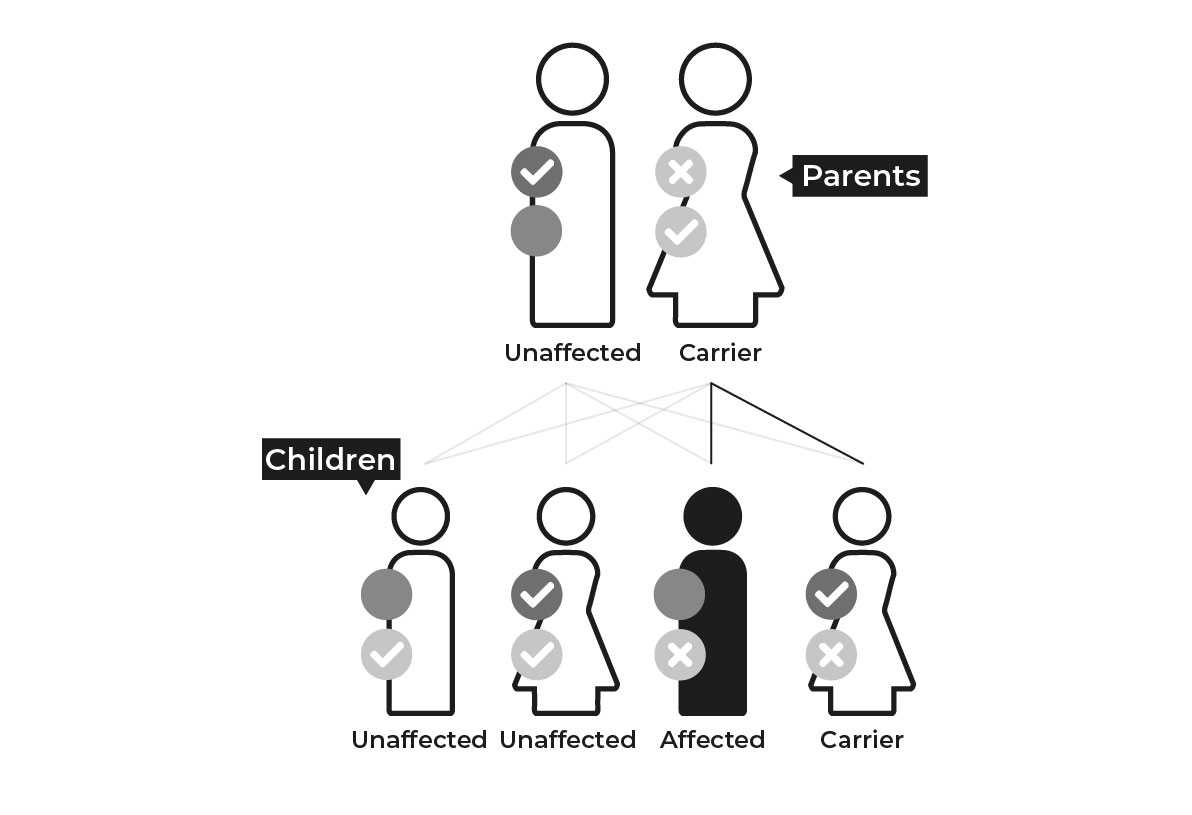
Autosomal: a mutation not linked to sex (X and Y) chromosomes
-
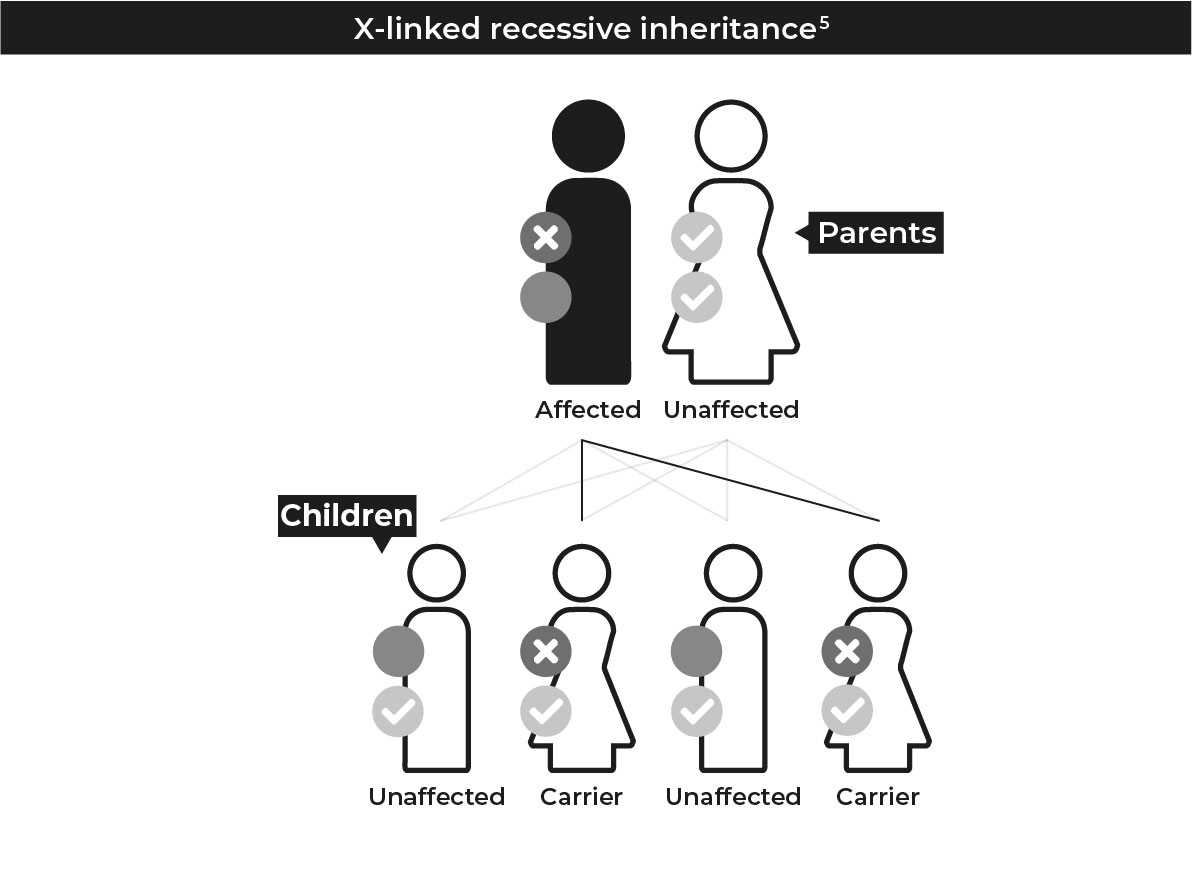
Allosomal: a mutation linked to sex (X and Y) chromosomes. Humans have one pair of sex chromosomes that determines biological sex; males have an X and Y chromosome while females have two X chromosomes
-
X-linked: a mutation that is on the X chromosome.
-
Recessive: means that you need two copies of the mutated gene for the disease to cause symptoms
-
Dominant: where only one copy of the mutation is needed for a person to be affected
-
Carrier: Someone who has a copy of a recessive mutation but is not affected by the disease associated with it. A carrier can pass the mutated gene on to their children
Inheriting IRD
You may wonder how you came to have an IRD. Different types of IRD have different inheritance patterns depending on the type of mutation and the gene(s) affected.
Humans have 46 chromosomes in 23 pairs containing all the genes that make us up. Each parent contributes one half of a chromosome paring. Below are the different ways that mutations that cause IRD can be inherited.
Common types of IRD
There are a lot of different conditions that together are called IRD. Many are named after the person who first described them. They can be caused by a mutation in one of over 260 genes that have been linked to these conditions.3
Types of IRD can be described as syndromic or non-syndromic. Syndromic IRDs are ones in which the eye problems are associated with other symptoms (such as hearing loss in Usher syndrome) as part of a systemic disease, whereas non-syndromic IRDs don’t have these systemic symptoms.6
Some of the more common IRDs are described below. As there are many others, you may have a type that isn’t included here. Other types of IRD can include: Bardet–Biedl syndrome, Joubert syndrome and primary ciliary dyskensia (among others).7
| Retinitis pigmentosa (RP)7,9 | ||
|---|---|---|
|
||
|
||
|
| Usher syndrome10 | ||
|---|---|---|
|
||
|
||
|
| Leber congenital amaurosis (LCA)11,12 | ||
|---|---|---|
|
||
|
||
|
| Stargardt disease13,14 | ||
|---|---|---|
|
||
|
||
|
Disease progression
Knowing the facts can put you at ease
The thought of your condition progressing can be unsettling, but knowing the facts and what to expect could help you to plan for your future.
How quickly an IRD is likely to progress and what symptoms you will develop can depend a lot on what form you have and the particular mutation. Even the same IRD can progress differently in different people. Many conditions start with difficulty seeing in low light levels, before leading to further vision problems. Loss of vision can be slow and gradual or can happen more suddenly. The different examples of visual impairment below help you to understand how the disease can develop.

Tunnel vision or loss of peripheral vision

Spots in the centre of vision

Blur in the centre of vision
Although your vision may worsen, there are a number of things you can do to help adjust and make changes so that IRD doesn’t stop you from living your life. See more in our section on Support and resources.
As IRDs can progress differently, it’s important to get the most accurate diagnosis you can. For more information on clinical diagnosis and genetic testing click here.
References
1. Retina International. Available at https://www.retina-international.org/educate/ Accessed February 2021. 2. Cremers FPM, et al. Genes 2018; 9(4): 215. 3. RetNet. Available at: https://sph.uth.edu/retnet/sum-dis.htm Accessed February 2021. 4. Hafler BP. Retina 2017; 37(3): 417–423. 5. Genetic Alliance. Understanding Genetics: A District of Columbia Guide for Patients and Health Professionals; District of Columbia Department of Health. Washington (DC): 2010 Feb 17. 6. Pierrottet CO, et al. Gen Med Res 2014; 13(4): 8833. 7. Berger W, et al. Prog Retin Eye Res 2010;29;335–75. 8. Menghini M, et al. Expert Opin Orphan Drugs 2020; 8(2-3): 67–78. 9. Sahel JA, et al. Cold Spring Harb Perspect Med 2015; 5(2): a017111. 10. Mathur P & Yang J. Biochim Biophys Acta 2015; 1852(3): 404–420. 11. Kumaran N, et al. Br J Ophthalmol 2017; 101: 1147–1154. 12. Chacon-Camacho OF, Zenteno JC. World J Clin Cases 2015; 3(2): 112–124. 13. Tsang T, Sharma T. Adv Exp Med Biol 2018; 1085: 139–151. 14.Tanna P, et al. Br J Ophthalmol 2017 Jan; 101(1): 25–30.
Recognising IRD
There are lots of different types of IRD and different tests doctors can carry out to work out which type you have.
Signs and symptoms
There are a range of different signs and symptoms that you might experience, beyond problems with your vision. These vary because of the number of diseases that are included in the term inherited retinal dystrophy. Below are signs of vision problems that might prompt a doctor to do more tests. This list highlights some of the problems you might see across different types of IRD.
In babies and young children:
-
Nystagmus (uncontrolled eye movements)1
-
Photophobia (sensitivity to light)1,2
-
Poking or rubbing of the eyes1
-
Problems with hearing and balance (mostly associated with Usher syndrome)3
In older children and teenagers:
-
Difficulty reading and seeing things at a distance
-
Loss of visual acuity2
-
Night blindness (nyctalopia) or problems seeing in dim or low light1,2
-
Slow eye response when switching from bright to dim light
This video gives an idea of what it can be like to live with an IRD, to care for someone who has it and also highlights some of the symptoms
How is IRD diagnosed?
Receiving a diagnosis for an IRD can be daunting, but knowing the process of a diagnosis is important in understanding your options.
There are two types of diagnosis for IRD: clinical diagnosis and genetic diagnosis.4

Clinical diagnosis
This is based on observations of the signs and symptoms you experience as well as tests in the doctor’s office. Its aim is to make a first diagnosis of an IRD, to find out what sort of IRD you have and what the likely course of your disease will be.
There are a number of different tests your doctor or ophthalmologist can carry out to see if you have an IRD and, if so, what sort it is. Some of these are outlined in more detail below.5

Genetic diagnosis
A genetic diagnosis is where genetic testing is used to tell you what gene mutation is causing your IRD. It’s used to validate and confirm the clinical diagnosis and find out exactly what is wrong. Not all of the mutations that cause IRD have been identified yet, but a large proportion have, and a genetic test should be able to tell you more.6,7
Clinical tests for IRD
Your doctor or ophthalmologist may carry out a number of different tests to diagnose IRD and work out which type you have. What might you expect?
Visual field testing: Uses a machine to check how much of the peripheral vision has been affected.8 This is non-invasive and involves you indicating when you can see a given stimulus, such as a flashing light, in your field of vision.8
Retinal imaging: Uses a special camera to take images of the back of the eye, including small structures and any abnormalities.9 This can be used to confirm a suspected clinical diagnosis and help guide further testing.
-
Fundus photography: A fundus photo is a picture of the retina that can be used to detect abnormalities. Fundus photography can be combined with autofluorescence imaging to give more information; it also makes it possible to diagnose Stargardt disease more easily.5
-
Optical coherence tomography (OCT): A scanning device that works by bouncing light waves off the retina to get a better picture of what is going on in the layers of the retina.5
Electroretinography (ERG): Measures the electrical response of rod and cone cells to light using an electrode placed on the cornea. This helps to see if the photoreceptor cells are functioning as they should be.5
Genetic testing
What is genetic testing?
Genetic testing involves looking at your DNA, usually from a blood sample, and sequencing your genes to find the specific mutations related to your IRD.8 It’s done to give a genetic diagnosis of your condition.8
Why is genetic testing useful?
Genetic testing can help to identify exactly what mutations are causing your IRD. This can help give a better idea of how your disease is likely to progress and can help guide your disease management. A genetic diagnosis can identify if you might be a candidate for any clinical trials or approved treatment (see more here) and can help provide information that can guide further research into the treatment of IRD.9
As well as this, a genetic diagnosis can help you to feel reassured about your condition, your likelihood of passing it on to your children, and how to manage your own disease.8
Getting referred for genetic testing
Your ophthalmologist or doctor will usually want to identify your IRD with a clinical diagnosis before proceeding to genetic testing. They may also want you to speak to a genetic counsellor before referring you for a test, so that you can receive help and support to make sense of your results.8
If you think a genetic test could be the right option for you, speak to your doctor about the possibility.
References
1. Kumaran N, et al. Br J Ophthalmol 2017; 101: 1147–1154. 2. Gill JS, et al. Br J Ophthalmol 2019; 103: 711–720. 3. Mathur P & Yang J. Biochim Biophys Acta 2015; 1852(3): 404–420. 4. Menghini M, et al. Expert Opin Orphan Drugs 2020; 8(2–3): 67–78. 5. Henderson RH. Paediatrics and Child Health 2019; 30: 1. 6. Hafler BP. Retina 2017; 37(3): 417–423. 7. Duncan JL, et al. Trans Vis Sci Tech 2018; 7(4): 6. 8. RNIB and RCOphth. Understanding Retinitis pigmentosa and other inherited retinal dystrophies. 2017. Available at: https://www.rnib.org.uk/eye-health/eye-conditions/ retinitis-pigmentosa Accessed February 2021. 9. Lee K, Garg S. Genet Med. 2015; 17(4): 245–252.
Back to top ^
Research into IRD
Ongoing research into treatments for IRD and how to get involved
IRD clinical trials – ongoing research
While there aren’t currently treatments available for many forms of IRD, there is a lot of research happening to try and find new options to treat these diseases. Most clinical trials are run at specialist centres and only include patients who have a particular diagnosis or specific genetic mutation, and some only run in specific countries. Most clinical trials across all different types of diseases are registered on the site, clinicaltrials.gov.
You can find a list of trials for treatments of inherited retinal dystrophy here.
Support and resources
Helpful information about IRD and what a diagnosis means for you.
You don’t have to deal with a diagnosis of IRD alone. Talk to your doctor about your options and what forms of support might be available to you in adjusting to life with IRD.
Other people are living with the same issues and adapting to life with IRD. There are patient support and advocacy groups out there who may be able to help you and where you can speak to people who are going through the same experiences as you. You can find some of these listed below.
Useful websites
Downloadable resources






